Advertisement
PCOS vs. Endometriosis: Causes, Treatments & How To Advocate For Yourself

When I first got my period at age 11, I thought I might be dying because of the horrid stabbing sensation. A decade later, I was finally diagnosed with endometriosis. Later still, tests confirmed a constellation of cysts on my ovaries, and doctors suspected I also had polycystic ovary syndrome, or PCOS, though I lacked many of the classic signs.
My experience is unfortunately common, as many people assigned female at birth now struggle with PCOS and/or endometriosis. Think you might be one of them? Let's walk through the differences and similarities between these two often debilitating conditions to help you talk to your doctor about your symptoms and navigate treatment—because those with PCOS or endometriosis shouldn't just have to "live with it" or "suck it up."
The need-to-knows:
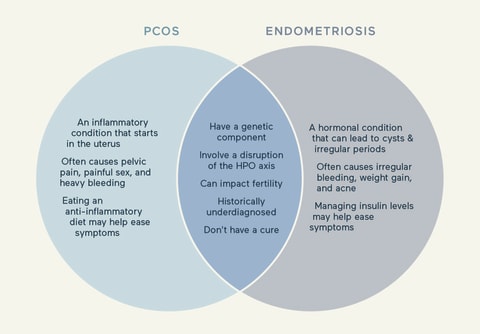
- PCOS vs. endometriosis: Endometriosis and PCOS are both common conditions among people assigned female at birth. They share some symptoms, (like fertility challenges) and it's possible to have both at the same time.
- They are both underdiagnosed: Many doctors (even OB/GYNs) are not knowledgeable about endometriosis or PCOS, leaving patients needing to advocate for themselves when they experience painful symptoms.
- Both PCOS & endometriosis deserve more attention—and research funding: We still don't know what causes PCOS or endometriosis, and we don't have a cure for either disorder. More resources need to be put toward researching them in the future.
What is PCOS?
"PCOS is a hormonal disorder that causes imbalances leading to enlarged ovaries and cysts1, irregular periods, and excess androgen levels, such as testosterone," says Shoma Datta-Thomas, M.D., an OB/GYN head of wellness at Modern Age.
PCOS affects 1 in 102 people assigned female at birth, meaning it's not rare. "PCOS is the most common endocrine condition in women during their reproductive years," says Nadia C. Brito Pateguana, B.Sc., N.D., with The Fasting Method. However, the World Health Organization reports that up to 70% of people with PCOS remain undiagnosed3.
PCOS can significantly affect quality of life and fertility1. It often puts people at an increased risk1 for other serious conditions, including Type 2 diabetes, cardiovascular disease, obesity, nonalcoholic fatty liver disease, cancer, mental health issues, and more.
Summary
Potential causes of PCOS
Researchers don't know the exact causes of PCOS, but it likely results from both genetic and environmental factors. However, let's be clear: PCOS is not the fault of the person with the condition. Here are a few potential causes:
- Epigenetics: Some research suggests that factors related to PCOS may be inherited4. People with a parent or sibling who has PCOS or Type 2 diabetes are more likely5 to have PCOS.
- Environmental toxins: Our environment is full of endocrine-disrupting chemicals. Concentrations of endocrine-disrupting chemicals tend to be higher4 in people with PCOS. These chemicals can mimic4 our hormones and act on their receptors, causing dysregulation. Bisphenol A, or BPA, is an example of a toxin that's prevalent in everything from plastics to dental fillings. BPA acts as an "obesogen," driving weight gain.
- Stress: Stress alone is likely not a direct cause of PCOS. However, it could be a contributor6 to metabolic issues related to PCOS, such as obesity, insulin resistance, and inflammation. And since chronic illness can leave you more stressed, PCOS and stress may be involved in a vicious cycle.
- Diet: Dysregulated glucose6, or blood sugar, is higher in people with PCOS. So is vitamin D deficiency4. Dietary changes7 have also been proven to help ease symptoms7 of PCOS. But when we talk about diet, we need to acknowledge issues with the food system. Globally, we've increased our consumption of ultra-processed foods8, which leads to dysregulated glucose. At the same time, rates of noncommunicable diseases related to dysregulated glucose are also going up. That's not a coincidence.
- Insulin resistance: Insulin resistance4 means that the body's cells have become less sensitive to insulin's signals to take in blood sugar. As a result, high insulin levels can occur. Insulin stimulates androgen secretion in the ovaries' theca cells, which can lead to issues with menstrual irregularities and fertility problems and further drive PCOS. Nearly 40% of U.S. adults have prediabetes, which is what insulin resistance is. However, doctors rarely treat prediabetes until it has become Type 2 diabetes.
- Hyperandrogenism: Hyperandrogenism4 means high androgen, or testosterone, levels. People with PCOS tend to have high testosterone levels. Higher testosterone can contribute to a cascade of issues that disrupt ovarian function and the menstrual cycle. High androgen levels also contribute to inflammation and oxidative stress. And while insulin resistance contributes to higher androgen levels, higher androgen levels can also contribute to insulin resistance, which can further fuel PCOS.
- Inflammation: PCOS is associated with higher markers of inflammation4, including a higher white blood cell count, a higher C-reactive protein level, and higher levels of pro-inflammatory cytokines. Inflammation can further drive insulin resistance and PCOS.
- Oxidative stress: Oxidative stress4 is an imbalance in the body between reactive oxygen species and antioxidants. This imbalance can cause cellular damage. Oxidative stress tends to be elevated in people with PCOS. Oxidative stress contributes to inflammation, insulin resistance, and obesity, all factors that can contribute to or exacerbate PCOS.
- Obesity: Obesity is connected to insulin resistance, oxidative stress, inflammation, and hyperandrogenism. Complex mechanisms involved in fat tissue4 drive PCOS, and PCOS is a driver of obesity.
Potential symptoms of PCOS
Symptoms of PCOS vary from person to person, but here are the most common presentations of the syndrome:
- Irregular menstrual cycle: Common menstrual irregularities9 associated with PCOS include missed or irregular periods, cramping, and more.
- Fertility issues: PCOS can halt or disrupt ovulation, causing difficulty with conception. It is the most common10 endocrine disorder that causes fertility issues in the female body.
- Excess facial and body hair: Hirsutism is known as male-patterned hair growth on the female body. Hirsutism is present in 70% to 80%11 of people with PCOS.
- Hair loss or balding: Alopecia, or hair loss, can also be a symptom, affecting about 40%12 of those with PCOS.
- Weight gain: Between 38% and 88%13 of people with PCOS have overweight or obesity. However, some people with PCOS are thin or lean14.
- Acne or oily skin: About three-quarters12 of people with PCOS also experience acne.
- Migraine: PCOS is associated with migraine15 attacks that occur before or during one's period or in general.
What is endometriosis?
Endometriosis is a chronic and painful inflammatory condition that is dependent on estrogen. Recently, the UK's National Health Service listed endometriosis as one of the top 20 most painful conditions.
The endometrium is tissue that lines the uterus and is shed each month during one's period. With endometriosis, tissue that "acts" like the endometrium16 implants on tissue outside the uterus.
There it forms lesions, or growths, on other tissues and organs. Since the lesions act like the endometrium, they respond to menstrual cycle hormones and bleed during one's period. The resulting internal bleeding can lead to scar tissue and adhesions, which can cause tissue and organs to "stick" together. For example, the bladder and uterus may become attached to each other.
"Something we've spent a lot of time on in the last several years is reimagining endometriosis as a systemic whole-body disease that affects multiple organs," says Hugh Taylor, M.D., a developmental biology professor and chair in the Department of Obstetrics, Gynecology, and Reproductive Sciences at Yale School of Medicine.
"It's not just a few lesions in the pelvis. It may start in the pelvis, but it has so many ramifications throughout the entire body that there's almost no organ that isn't affected," Taylor adds. Lesions also secrete proteins called pro-inflammatory cytokines17, leading to inflammation and pain, which can be debilitating.
Summary
Potential causes of endometriosis
Researchers don't yet know the exact causes of endometriosis, but they do have some theories:
- Retrograde menstruation: Retrograde menstruation20 is when menstrual fluid passes through the fallopian tubes and into the pelvic area. Endometrial cells can then implant, leading to tissue that mimics the endometrium. Almost all, 90%20, of people assigned female at birth have some degree of retrograde menstruation. "It's a balance of how much your body can clear it and how likely it is to implant," Taylor says. Researchers note that this theory20 needs to be further explored for more understanding.
- Genetics: Endometriosis may be inherited. Many people with endometriosis have a first-degree relative21 with the condition. But more research is needed.
- In-utero exposure: Some research links exposure to certain medications or chemicals during gestation22 to the development of endometriosis.
- Environmental toxins: Endocrine-disrupting chemicals in the environment, also called "obesogens," may be to blame for causing endometriosis. For example, dioxins22, which are industrial pollutants, are found at higher levels in people with the condition.
- Immune system issues: Research points to immune-system involvement, but more research is needed. Cytokines are molecules that help regulate the immune system. But an overabundance can be problematic. Endometriosis lesions secrete23 pro-inflammatory cytokines. Endometriosis is also associated24 with several autoimmune disorders, including lupus, rheumatoid arthritis, celiac disease, multiple sclerosis, and inflammatory bowel disease. And endometriosis tends to be more severe25 in people with autoimmune dysfunction. Endometriosis is not currently classified as an autoimmune disorder. "Altered immune system and autoimmune disease is certainly a component of endometriosis," Taylor says, "but it's not the whole story."
- High estrogen levels: High estrogen26 production is a consistent characteristic of people with endometriosis. And estrogen fuels endometriosis lesions, inflammation, and pain.
- Diet: Diet is not a cause of endometriosis, but diet may play a role in the disease expression. Diet affects sex hormones22 and can impact levels of inflammation. Of note, a diet featuring a lot of red meat may increase endometriosis risk22, whereas a diet high in fruits and vegetables may decrease the risk.
Potential symptoms of endometriosis
Endometriosis can cause the following symptoms:
- Pelvic pain: Pain27 is one of the most common features of endometriosis. However, not everyone with the condition experiences pain. And pain can result from just a few endometriosis lesions. Endometriosis-related pelvic pain is common just before and during one's period. However, it may occur at any time. Pain elsewhere in the body, such as in the back, hips, and legs, is also common with endometriosis.
- Pain with sex: People with endometriosis have a nine-fold increase in the risk of dyspareunia, pain with intercourse.
- Pain with bowel movements or urination: Endometriosis can affect the bowel or bladder28 and may cause discomfort with going to the bathroom.
- Gastrointestinal symptoms: In addition to pain, people with endometriosis often experience gastrointestinal issues29, such as constipation, diarrhea, nausea, bloating, SIBO, and more.
- Heavy bleeding: Having heavy periods30 and bleeding when you're not on your period are also common endo symptoms.
- Fertility issues: About 30% to 50%31 of people with an endo diagnosis have trouble with fertility.
- Migraine: More than 50%32 of people assigned female at birth with migraine report that their attacks occur near or around menstruation, and migraine and endometriosis have strong links32.
- Ovarian cysts: People with endometriosis may also experience ovarian cysts called endometriomas. These cysts, resulting from endometriosis, are filled with endometrial-like fluid and are sometimes called "chocolate cysts." About 17% to 44%33 of people with endometriosis will develop endometriomas.
- Increased sensitivity to pain: "We know endometriosis changes and remodels the brain," Taylor says. "We've done that in animal studies. We give mice endometriosis. We look at their brains. Their electrophysiology is different. Their gene expression is different. Their behaviors become different within a few weeks of getting the endometriosis. And they become more pain sensitive to the same painful stimuli."
- Anxiety and depression: People with endometriosis are often told that their pain symptoms are a result of anxiety or depression. "It's the exact other way around," Taylor says. "These conditions of the brain are caused by endometriosis." Taylor says mice develop depression and anxiety when endo is induced in their bodies, even in the absence of pain.
- Low BMI: In the past, doctors have blamed endometriosis on being too thin because many people with the condition have a low BMI, Taylor says. However, that's not a cause. "[Endo] affects your fat cells," he adds. "It affects your liver34 and changes your metabolism to cause weight loss." He notes that not everyone with endometriosis is thin, however.
Diagnosing PCOS and endometriosis
PCOS:
In order to diagnose PCOS, doctors use a combination of pelvic imaging, blood tests, and other exams. "It is a syndrome and a diagnosis of exclusion, which requires extensive testing," says Pateguana. A diagnosis of exclusion means doctors must rule out other potential causes of symptoms first.
Some boutique clinics like Modern Age now offer specialty tests that measure over 50 biomarkers and may prove useful in identifying potential risk factors for PCOS.
Endometriosis:
Endometriosis has historically been diagnosed with laparoscopic surgery16—a small camera is inserted into the abdomen to look for lesions. However, this isn't the only diagnostic method we have, and some physicians (like Taylor) advocate for nonsurgical diagnosis35.
"We can make a presumptive diagnosis by listening to our patients and considering all these symptoms and putting the pieces of the puzzle together," he says. "If you wait to require surgery to make a definitive diagnosis, you're waiting until somebody's really miserable. And that's just cruel in my mind. It's really held people back for years and disrupted their lives before they get adequate treatment."
However, many people with suspected endometriosis, whom I've interacted with, prefer a definitive surgical diagnosis because it helps them advocate for themselves at the doctor's office.
Why the delays in receiving a diagnosis for PCOS and endometriosis?
People often experience delays of multiple years in receiving a diagnosis for endometriosis and PCOS36.
Why is that? For endometriosis, researchers note a lack of health care provider knowledge and a lack of adequate research funding37 for the condition. The National Institutes of Health designated less than 0.1% of research funding38 to studying endometriosis in 2022.
A diagnosis of PCOS may be delayed because of a lack of provider education as well. Symptoms also overlap with other health issues, which can further complicate and delay diagnoses. "Age-related factors can also affect symptom perception, emphasizing the need for preventative health care," says Datta-Thomas.
Menstrual cramps are the only pain we as human beings ever accept as a 'normal' pain you’re supposed to have.
Let's not forget that patients with PCOS and/or endometriosis also report not having their symptoms taken seriously when they take them to their doctors. Medical gaslighting, which women are disproportionately affected by, is common with both conditions.
I remember one doctor, in 2007, despite clear surgical evidence (from multiple procedures) of my endometriosis, walked into my hospital room and said, "Don't you think it's all up here?" while she pointed to my head.
Another issue is the inappropriate normalization of pelvic pain. "Many patients initially have their pain dismissed and told, or it's insinuated, that they're weak and they're not able to tolerate normal menstrual cramps—when that's just not the case," Taylor says. "Menstrual cramps are the only pain we as human beings ever accept as a 'normal' pain you're supposed to have."
Real-life stories
What are the differences between PCOS and endometriosis?
Endometriosis and PCOS are two different chronic conditions with different causes and symptoms, though some overlap. Endocrine-disrupting chemicals are implicated as a potential cause in both conditions, for example. And fertility issues are another commonality.
According to recent research, both conditions involve disruption39 of the hypothalamic-pituitary-ovarian axis. The HPO axis is the feedback loop that controls the menstrual cycle. This disruption may occur in utero to the fetus.
Research, including animal studies, suggests that high levels of prenatal testosterone fuel the development of PCOS, while low levels of prenatal testosterone may lead to the development of endometriosis. But we need more studies.
Can you have both endometriosis and PCOS at the same time?
A key difference between the two is that estrogen drives endometriosis, while testosterone drives PCOS. "High testosterone levels can actually suppress endometriosis," Taylor says. "But they're not usually high enough in PCOS to do that. Not everyone with PCOS has very high testosterone levels. And there's usually enough estrogen around in PCOS to grow endometriosis as well."
"Women with insulin resistance may also have a higher incidence of inflammatory conditions such as endometriosis," Pateguana adds. And insulin resistance is a significant component of PCOS.
Navigating fertility with PCOS and/or endometriosis
Fertility issues are common to both endometriosis and PCOS. However, various treatments and strategies can help boost fertility.
"Endometriosis' effects on fertility are not completely understood but likely involve inflammatory pathways and anatomic damage," Datta-Thomas says. "It may cause scarring and affect the reproductive organs, which has an impact on fertility for many women."
Surgery31 may be necessary to remove lesions and address anatomical issues. And additional fertility assistance may be necessary. "If endometriosis has scarred the tubes, then a woman will often need IVF," says functional gynecologist Wendie Trubow, M.D., MBA.
"PCOS can impact fertility, as it involves hormonal imbalances that affect the regularity of ovulation and, in some cases, lack of ovulation, which can make it challenging to conceive," Datta-Thomas adds. "Addressing these conditions through timely diagnosis and management can positively influence fertility outcomes, and effective management of these conditions not only contributes to fertility but also supports overall health and longevity."
Treatment options for PCOS
PCOS does not have a cure but can be treated and managed in various ways, including the following:
- Medication
- Surgery
- Nutritional changes
- Exercise
Here's a little more on each route:
Medication & surgery:
"The conventional treatment for PCOS," Pateguana says, "is the birth control pill to help regulate cycles and other Band-Aid treatments to treat each symptom (there are often many symptoms and expressions) as well as fertility treatments to attempt successful pregnancy, but none of the current conventional treatments reverses PCOS."
If obesity, and/or Type 2 diabetes, is present, weight loss medications, such as glucagon-like peptide 1 receptor agonists (such as Ozempic and Wegovy) may help40. First-line blood-sugar-lowering meds, such as metformin41, might be prescribed for those with insulin resistance. Weight loss surgery42 may also be a consideration for those who are candidates.
Nutritional changes:
Ultimately, the latest research shows that addressing and managing insulin resistance is key since it's such a huge factor in PCOS. Plus, we have natural ways of managing insulin resistance. To become more insulin sensitive, which is a good thing, Pateguana has some advice.
"The main tip is to focus on reversing metabolic syndrome and lowering insulin through fasting and a low insulin diet (aka low carb)," she says. A ketogenic diet has been shown to be helpful43 in managing symptoms, for example.
Some people choose to wear a continuous glucose monitor to track blood sugar, keep their glucose levels more stable, and learn what foods cause glucose spikes. (I did this for a month and the experience was eye-opening, especially for the banana and oat milk I used to put in my smoothie!) High blood sugar drives insulin resistance. However, mitigating blood sugar spikes helps to reverse insulin resistance, which could help with PCOS.
Additionally, avoiding ultra-processed foods as much as possible, in favor of whole foods, helps support your overall metabolic health.
Exercise:
Treatment options for endometriosis
Like PCOS, endometriosis does not have a cure—nope, not even hysterectomy. However, endo can be managed with various treatment options and strategies, including the following:
- Medication
- Surgery
- Lifestyle changes
Medication:
Typically, the goal of treatment involves pain management and maintaining the health of various organs, especially in the pelvis.
"The first-line treatment is birth control," Taylor says, "not because it's the best or greatest but because it's easy and people are familiar with it." Hormonal birth control helps in about one-third of people with endometriosis, according to Taylor.
"But there are a lot more people who have side effects from birth control pills," he adds. "For about half of women, it either doesn't work to relieve pain, or they stay on it because it's helping with the pain, but they feel terrible in other ways."
Another medication used to treat endometriosis is Lupron, which induces medical menopause. However, Taylor notes the issues with this medication, which was frequently prescribed in the past45. It has fallen somewhat out of favor now. He describes it as "a very harsh injectable drug that's slow to act and actually can, for the first couple of weeks, make the disease worse before it gets better."
I personally took one injection of this medication in 2002, and it was a horrid experience that required me to take a quarter off graduate school.
Also under the list of medication treatments is gonadotropin-releasing hormone agonists46, or GnRHa meds. "Orilissa and Myfembree are the brand names that are of a milder or gentler form that are oral, that work right away." These drugs reduce estrogen levels to help combat endometriosis, he explains.
A host of medications may also be prescribed to help manage pain, including anticonvulsants and pelvic floor Botox. Meds, such as antidepressants47, may also be prescribed to help manage the mental health symptoms endometriosis causes.
None of the medication treatments will help with fertility, however, because they suppress the hormones that are necessary for pregnancy, Taylor adds.
Surgery:
Many people with endometriosis require surgery to remove lesions and endometriomas and to fix anatomical issues. Anatomical issues can involve adhesions48 that are causing organs to stick together or issues like an incarcerated uterus49. An incarcerated uterus is when the womb is retroverted50, meaning it's tipped backward and is stuck in that position. Endometriosis lesions can cause a uterus to become incarcerated.
"None of these treatments address the inflammatory component of endometriosis," Taylor says. He is quick to add that researchers need to come up with better treatments for endometriosis and that his team at Yale has new treatments in the pipeline.
Lifestyle changes:
Finally, lifestyle changes may also help manage endometriosis. Eating an anti-inflammatory diet may be of benefit51, for example. Sugar itself and high-carbohydrate diets drive inflammation, as do ultra-processed foods. Eating whole, organic foods may be able to help and support your gut microbiome and therefore your immune system.
Both Trubow and Pateguana are also advocates for acupuncture to help with endometriosis pain. Although we need more research on acupuncture, one small study noted a 62% reduction in pain52 for participants with endometriosis.
Finally, if you have pain with sex, talk to your doctor about it. They may be able to refer you to a physical therapist who can help with pelvic floor dysfunction53, which is linked to endometriosis.
In my case, I was finally granted a hysterectomy with removal of my cervix, tubes, and left ovary, as well. My uterus had anatomical issues, and my left ovary was enlarged and frequently cystic. I'm happy to report that the procedure brought immense pain relief. However, it's not the right solution for everyone, and I do still have endometriosis and related symptoms.
Advocating for yourself
Whether you have endometriosis, PCOS, or both conditions, the importance of advocating for yourself at the doctor's office cannot be understated. The first thing to know is that symptoms aren't in your head, and, no, you shouldn't just have to deal with the pain or other issues.
Taylor acknowledges the "demeaning" things the medical community has said to people assigned female at birth with these conditions. He wants people to know that menstrual cramps should not change or get worse over time. If your doctor is dismissing your symptoms, he advocates for speaking up or finding a doctor with expertise in endometriosis or PCOS if possible.
For some tips on how to advocate for yourself, which I acknowledge isn't always easy, I reached out to Abby Norman, the author of Ask Me About My Uterus: A Quest To Make Doctors Believe in Women's Pain. Here is her advice:
- Be specific about your symptoms.
- If you have support, bring someone along to your doctor's appointment.
- If you don't have personal support, some hospitals and community health centers have advocates who can help.
- Teach back. Before you leave, repeat to your doctor what they've said to you to help aid in clarity.
- Review your after-visit summary. "Administrative staff are human," Norman says, "and they do make mistakes. But even 'slight' medical errors can have major consequences." Reach out if you notice errors!
- Request copies of your medical records and share them with your health care team, especially if you're seeing separate doctors from multiple health systems.
A tip from me: Don't be afraid to fire your doctor and request a different one within your network. I can't even count how many doctors I've canned and reported for their incompetence and inappropriate comments over the last two decades. I recognize that finding a different doctor within network may not always be possible. However, you always have the right to speak up and express your concerns.
The mindbodygreen POV
PCOS and endometriosis are both extremely common—but unfortunately, difficult to get a proper diagnosis for. As covered in this piece, there are some key differences between PCOs and endometriosis but also a few similarities, and they can both exist simultaneously in rare cases. If you suspect you have either or both, share your symptoms with your doctor. As Jennifer's experience shows, finding the right treatment plan can be a long and frustrating journey. Know that you're not alone—and many people are suffering from the same symptoms. Visit our Invisible Illness series for more advice on advocating for yourself when you have a chronic health condition.
—Emma Loewe, mindbodygreen Health & Sustainability Director
FAQ
How do I know if I have endometriosis or PCOS?
See your doctor. PCOS is diagnosed with various tests, and endometriosis is often diagnosed with surgery, though other tests and exams are also used.
What's more painful, endometriosis or PCOS?
Both conditions can involve pelvic and other types of pain, but pain is more prevalent with endometriosis.
Can PCOS cause endometriosis?
PCOS is not the cause of endometriosis; however, they can exist together.
The takeaway
Endometriosis and PCOS are both common conditions that can wreak havoc on whole-body health and well-being. They can occur separately or together, and neither has a cure. However, some treatments can help with condition management.
Researchers acknowledge we need better treatments, and that symptoms from these conditions should be taken seriously and addressed. Unfortunately, not all doctors, even OB/GYNs, are knowledgeable about endo or PCOS. Thus, people assigned female at birth are often left to advocate for themselves.
As someone who lives with endometriosis and has experience with PCOS, I continue to be hopeful that researchers will develop better treatments for both conditions so that others like me will be spared pain, medical debt, and emotional turmoil in the future.
53 Sources
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4820451/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8288001/
- https://www.who.int/news-room/fact-sheets/detail/polycystic-ovary-syndrome
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8775814/
- https://www.cdc.gov/diabetes/basics/pcos.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8771268/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8643565/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10058108/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5562990/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3108690/
- https://pubmed.ncbi.nlm.nih.gov/27510481/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8451069/
- https://journals.sagepub.com/doi/full/10.1177/1179558119874042
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6405408/
- https://link.springer.com/article/10.1007/s11033-021-06799-8
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9537113/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6737540/
- https://www.who.int/news-room/fact-sheets/detail/endometriosis
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5833878/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8508982/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6447774/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8582818/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9265783/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6601386/
- https://www.nature.com/articles/s41598-021-94877-z
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7215544/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7573391/
- https://www.ncbi.nlm.nih.gov/books/NBK279502/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4535676/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4287196/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7559069/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9290099/
- https://www.ncbi.nlm.nih.gov/books/NBK559230/
- https://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(21)00389-5.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10120420/#:~:text=Although%20surgery%20can%20provide%20a,reduce%20delays%20to%20starting%20treatment.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6283441/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9537113/#REF102
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9127440/#:~:text=Research%20funding%20for%20endometriosis%20is,and%20over%20190%20million%20worldwide.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9361725/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9405922/
- https://www.cureus.com/articles/167371-role-of-metformin-in-polycystic-ovary-syndrome-pcos-related-infertility#!/
- https://www.mdpi.com/2077-0383/12/12/3940#:~:text=Polycystic%20ovary%20syndrome%20(PCOS)%2C,Y%20gastric%20bypass%20(RYGB).
- https://pubmed.ncbi.nlm.nih.gov/32103756/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7358428/
- https://pubmed.ncbi.nlm.nih.gov/2118858/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10201290/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8779548/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6334013/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8924533/
- https://www.sciencedirect.com/topics/medicine-and-dentistry/uterine-retroversion
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9983692/
- https://pubmed.ncbi.nlm.nih.gov/18794019/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5585080/
Watch Next
Enjoy some of our favorite clips from classes
Enjoy some of our favorite clips from classes
What Is Meditation?
Mindfulness/Spirituality | Light Watkins
Box Breathing
Mindfulness/Spirituality | Gwen Dittmar
What Breathwork Can Address
Mindfulness/Spirituality | Gwen Dittmar
The 8 Limbs of Yoga - What is Asana?
Yoga | Caley Alyssa
Two Standing Postures to Open Up Tight Hips
Yoga | Caley Alyssa
How Plants Can Optimize Athletic Performance
Nutrition | Rich Roll
What to Eat Before a Workout
Nutrition | Rich Roll
How Ayurveda Helps Us Navigate Modern Life
Nutrition | Sahara Rose
Messages About Love & Relationships
Love & Relationships | Esther Perel
Love Languages
Love & Relationships | Esther Perel
What Is Meditation?
Box Breathing
What Breathwork Can Address
The 8 Limbs of Yoga - What is Asana?
Two Standing Postures to Open Up Tight Hips
How Plants Can Optimize Athletic Performance
What to Eat Before a Workout
How Ayurveda Helps Us Navigate Modern Life
Messages About Love & Relationships
Love Languages
Advertisement

Your Grandma's Go-To Supplement Is Once Again Popular (For A Good Reason)
Molly Knudsen, M.S., RDN

This Type Of Fat Is Vital For Women's Health — Are You Getting Enough?
Molly Knudsen, M.S., RDN

New Study Confirms The 3 Habits That Age Your Brain Faster
Molly Knudsen, M.S., RDN

Your Grandma's Go-To Supplement Is Once Again Popular (For A Good Reason)
Molly Knudsen, M.S., RDN

This Type Of Fat Is Vital For Women's Health — Are You Getting Enough?
Molly Knudsen, M.S., RDN

New Study Confirms The 3 Habits That Age Your Brain Faster
Molly Knudsen, M.S., RDN